A comprehensive new survey from KFF and The New York Times offers critical insight into how heightened immigration enforcement is reshaping healthcare access patterns — and what it means for language access programs.
The survey, conducted among 1,805 immigrants nationwide between August and October 2025, reveals measurable shifts in healthcare utilization and patient behavior that have direct operational implications for health systems. For language access leaders navigating resource allocation, program planning, and quality outcomes, these findings warrant close attention.
Healthcare Avoidance Is Rising
The data shows a clear trend: immigrants are increasingly delaying or skipping medical care.

29% of immigrants reported skipping or postponing healthcare services in the past 12 months — up from 22% in 2023. Among those who deferred care, the reasons are telling:
- 63% cited cost or lack of insurance
- 42% couldn't find services at a convenient time or location
- 24% of non-English speakers couldn't access care in their preferred language or obtain an interpreter
- 19% were concerned about immigration status
Perhaps most concerning: 36% of those who skipped care reported that their health worsened as a result. This deferred care doesn't disappear — it can often resurface as more acute, more complex, and more costly interventions.
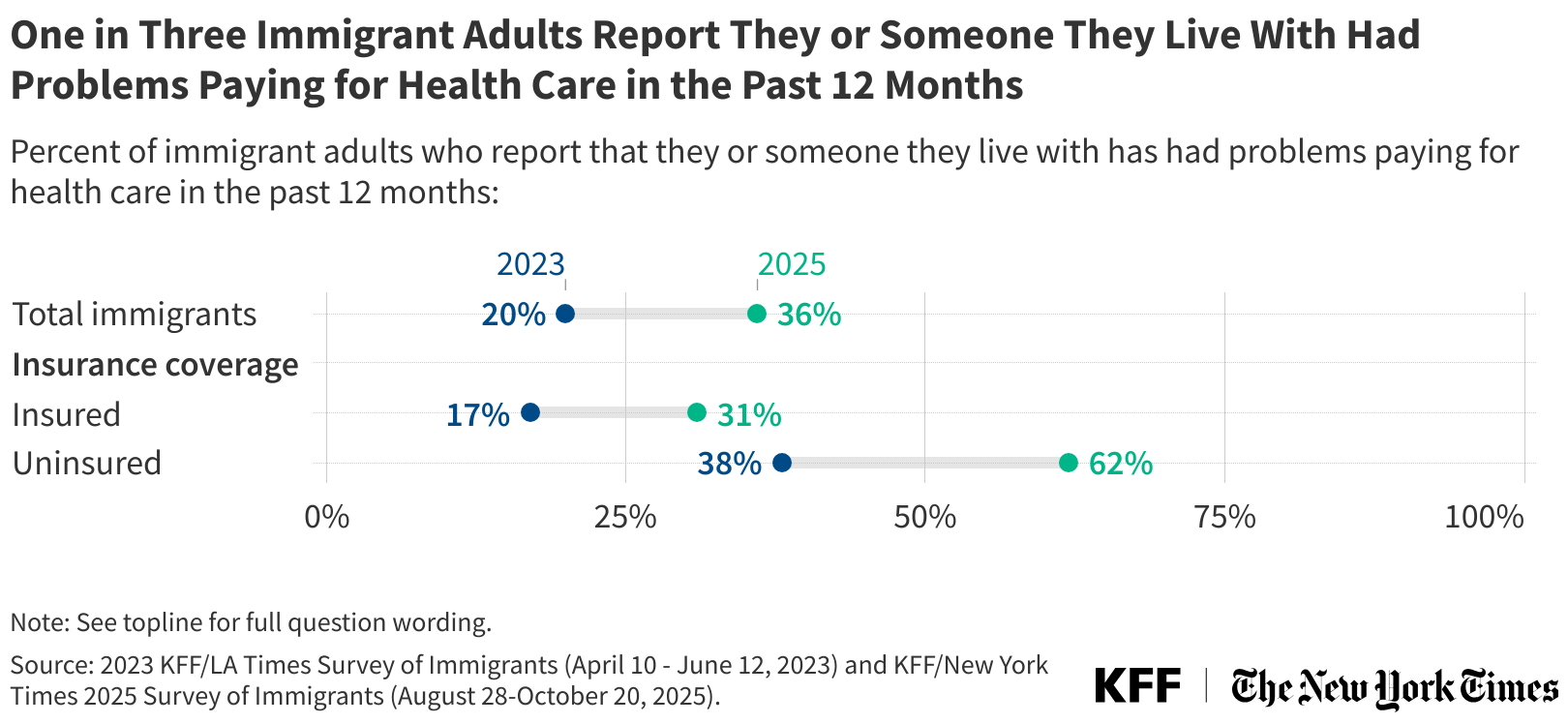
Financial Strain Is Intensifying
The survey reveals significant increases in financial hardship among immigrant populations:
- 36% had problems paying for healthcare (up from 20% in 2023)
- 30% had problems paying rent or mortgage (up from 17%)
- 27% had problems paying for food (up from 17%)
Nearly half of all immigrants — 47% — reported struggling to pay for at least one of these basic needs, compared to 34% two years ago.
When patients face these pressures, healthcare utilization patterns shift: non-urgent care gets postponed, prescriptions go unfilled, and follow-up appointments are missed. On top of being patient experience issues, these are operational and clinical performance issues that show up in length of stay, readmission rates, and quality measures.
Trust Erosion Creates New Barriers
Beyond financial strain, the survey identifies a trust crisis that directly affects healthcare access.
51% of immigrants expressed concern about health officials, hospitals, or healthcare providers sharing patients' immigration status with federal enforcement agencies. This concern exists across immigration statuses — it's not limited to undocumented immigrants.

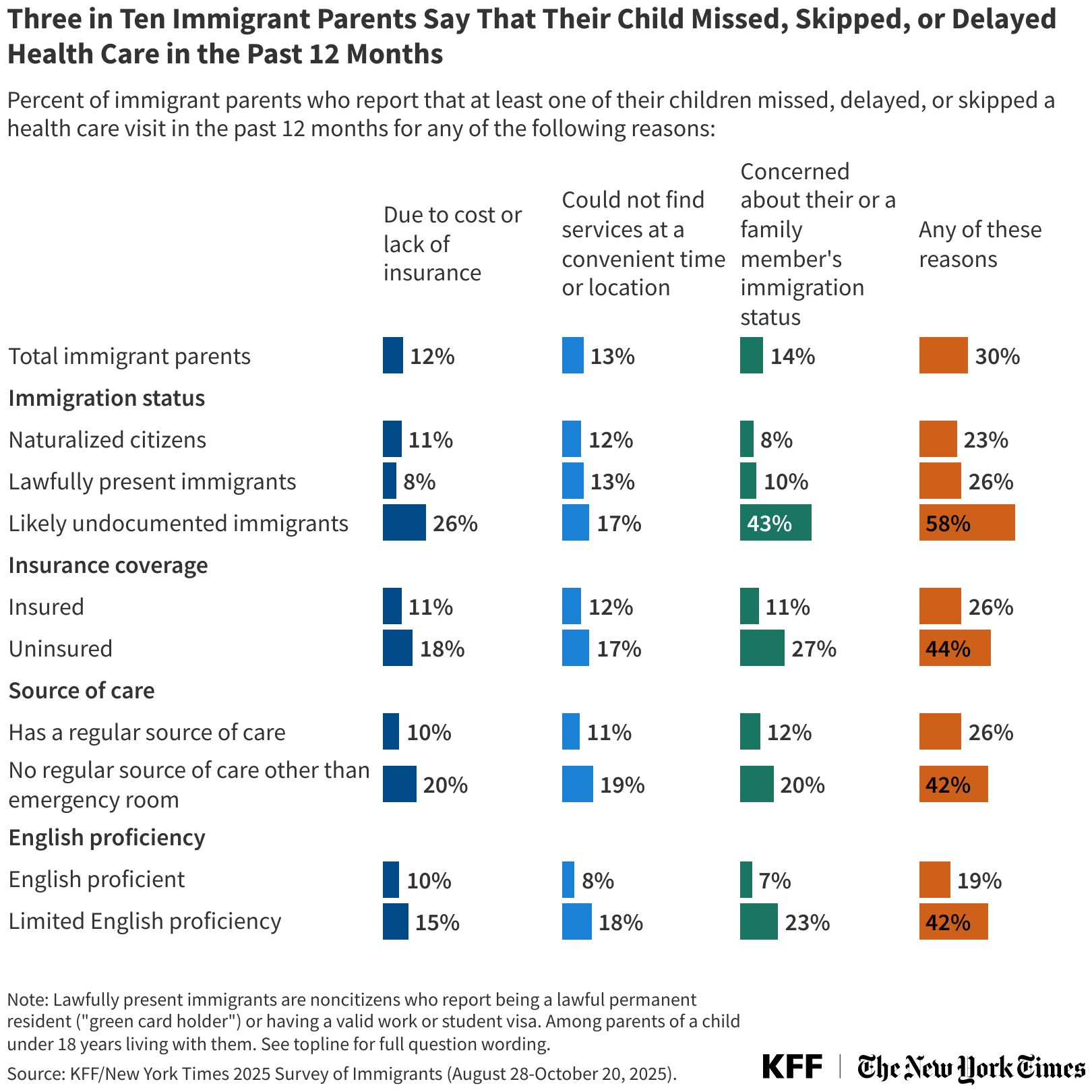
14% of immigrants reported avoiding medical care specifically due to concerns about drawing attention to immigration status. Among parents, 14% said their children missed, delayed, or skipped healthcare for the same reason.
When institutional trust erodes, language access becomes even more critical. Professional medical interpreters serve as trusted intermediaries in the care delivery process, particularly when patients are weighing whether to seek care at all.
What This Means for Language Access Programs
These findings have several implications for how language access programs function during periods of heightened immigration enforcement:
Utilization patterns may shift unpredictably. When fear drives healthcare avoidance, traditional demand forecasting becomes less reliable. Emergency departments may see different acuity mixes. Scheduled appointments may have higher no-show rates. Discharge planning may face new complications when patients are reluctant to engage with follow-up care.
Language access quality becomes a trust signal. When patients are weighing whether to seek care, every interaction matters. The presence of qualified medical interpreters — who understand healthcare terminology, HIPAA protections, and cultural context — reinforces that the healthcare environment is safe and confidential. By contrast, gaps in language access or reliance on ad hoc interpreters can amplify patient reluctance to engage with care.
Deferred care creates downstream cost and quality impacts. As the survey shows, delayed care often means worsening health. For health systems, this translates to higher acuity at presentation, longer lengths of stay, more complex care coordination, and increased readmission risk — all metrics that language access programs are positioned to influence through clear, consistent communication.
Documentation and compliance take on added importance. In an environment where 51% of immigrants worry about information sharing, clear documentation of interpreter services, HIPAA compliance, and patient privacy protections becomes both an operational necessity and a patient reassurance tool.
Moving Forward
At Martti, we're monitoring utilization patterns across our partner health systems and continuously modifying interpreter availability in accordance with shifting demand. The goal is to ensure that when patients do seek care — despite their fears — language barriers don't compound the challenge.
For language access leaders, these survey findings underscore a reality that goes beyond compliance: language access is infrastructure for trust, safety, and equitable care delivery. When that infrastructure is reliable, responsive, and high-quality, it supports better outcomes for patients and stronger operational performance for health systems — particularly during periods of uncertainty.
The data is clear, the operational implications are real, and the need for strategic, well-resourced language access programs has never been more urgent.










