By Maureen Huber, CEO
Every hospital executive knows the stakes of patient communication.
But at our early-morning roundtable in Chicago during Becker's 10th Annual Health IT + Digital Health + RCM Conference last week, the conversation revealed just how much higher the stakes have become.
Roundtable Speakers:
Dean M. Harrison, our board member and the former CEO of Northwestern Medicine, framed it well.
“Language access in a hospital is like water,” he said. “It needs to be there when you need it, and it needs to work.”
In healthcare, we don’t congratulate ourselves for running water. We notice it only when it fails, and by then, everything else is failing too.
Part of that is because communication failures create frustration, but that’s only part of the picture.
They drive avoidable safety events, longer hospital stays, costly readmissions, and break down trust between patients and clinicians.
In a healthcare environment already stretched by workforce strain and financial pressures, these are failures we cannot afford.
In sum, treat compliance as the minimum, build language access into the bones of care, and help clinicians use it without friction.
Here are the key takeaways.
The Five Foot Rule
Here’s the humbling truth: language access fails by inches.
We know that if a Martti-enabled device sits more than five feet from where a conversation is happening, it is less likely to be used.
Five feet – hardly anything on a floor plan – becomes the distance between intention and equity.
The tools that empower our communication need to live exactly where care happens. When they do, utilization rises. When they don’t, policies stay stuck on paper and communication barriers exist.
We kept returning to the same conclusion: build language access into clinical workflows (physical and digital) or it won’t be there when it’s needed.
Integrating Language Services is Key
Gaps in access exist across the care continuum.
Here are a few examples:
✖ Education and training of staff is inconsistent and insufficient
✖ A device that isn’t where it should be
✖ Interpretation access buried five clicks deep in the EHR
✖ Telehealth solutions without integrated access
But, if you manage to integrate language services into your clinical workflows, adoption follows.
At the roundtable, we talked about interpreter presence at consent and discharge, and the mix of in-person, VRI, and OPI, because those are the measures that change behavior.
Finding the Patient-Experience Sweet Spot
AI-enabled interpretation is the natural next step of interpretation technology.
Ryan Beauchamp, Managing Director & Head of Product & AI at GTCR, who advises on emerging technology, offered a compass: aim for the patient-experience sweet spot.
The Human–AI Spectrum in Medical Interpretation:
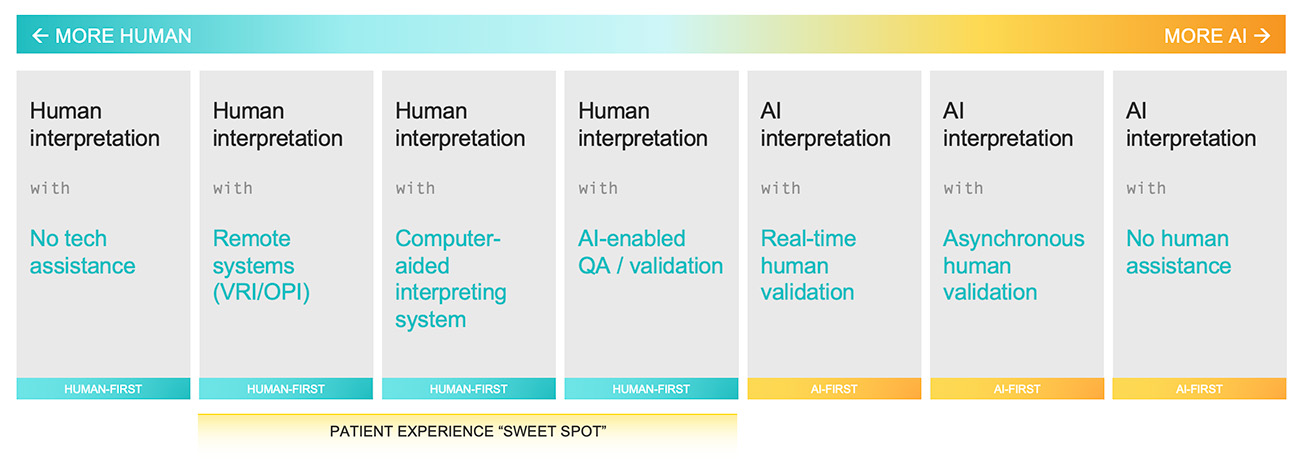
Use AI where it reliably speeds access and consistency, like documentation support, captioning, and quality review. Then, draw a line at the moments that depend on cultural nuance and trust, such as consent, delivering medical information, and complex decision-making, to name a few.
In other words, deploy technology where it enables human interpreters to be more present, not less.
That “sweet spot” (highlighted in the image above) exists on a spectrum. It’s more human on one end, more AI on the other, and the sweet spot for medical interpretation is human-first, with AI assisting, not replacing.
Compliance as the Floor, Not the Ceiling
Meeting federal and state requirements is non-negotiable, but compliance alone isn’t enough.
Boards and CEOs want proof that risk is being proactively managed, not simply avoided.
Our presentation called this out plainly: reduced length of stay and readmissions, improved safety and HCAHPS, greater equity, and stronger patient trust.
Education and Workforce Adoption
Even the best technology and the most robust policies fail if frontline staff aren’t trained and supported.
Staff education must go beyond compliance modules. It requires ongoing coaching, champions, and visible support from leadership.
Empowering clinicians to use language services confidently is what closes the gap between policy and patient experience.
What the Room Made Clear
The roundtable reinforced what I believe deeply: language access is critical infrastructure for equitable, safe, high-quality care.
The fact that compliance, integration, and education rose so quickly to the top means health systems see both the risks and the opportunities. The next step is execution – turning those themes into enterprise commitments, improving key performance indicators and building patient trust.
Want to learn more about the roundtable? Contact us.










