Two recent studies reveal a troubling intersection: at a time when immigrants are increasingly avoiding in-person healthcare due to safety concerns, patients with limited English proficiency face significant barriers to accessing the virtual care that could help address those fears.
The convergence of these trends has urgent implications for language access programs navigating both patient safety and health equity.
Two parallel realities
A comprehensive survey from KFF and The New York Times, conducted among 1,805 immigrants nationwide between August and October 2025, documented rising healthcare avoidance driven by fear and institutional distrust.
Key findings include:
- 29% of immigrants skipped or postponed medical care in the past 12 months, up from 22% in 2023. Among those who deferred care, 36% reported their health worsened as a result.
- 51% of immigrants expressed concern about healthcare providers sharing immigration status with federal enforcement agencies. This concern exists across all immigration statuses, not just undocumented immigrants.
- 14% avoided medical care specifically due to concerns about drawing attention to immigration status. Among parents, 14% said their children missed, delayed, or skipped healthcare for the same reason.
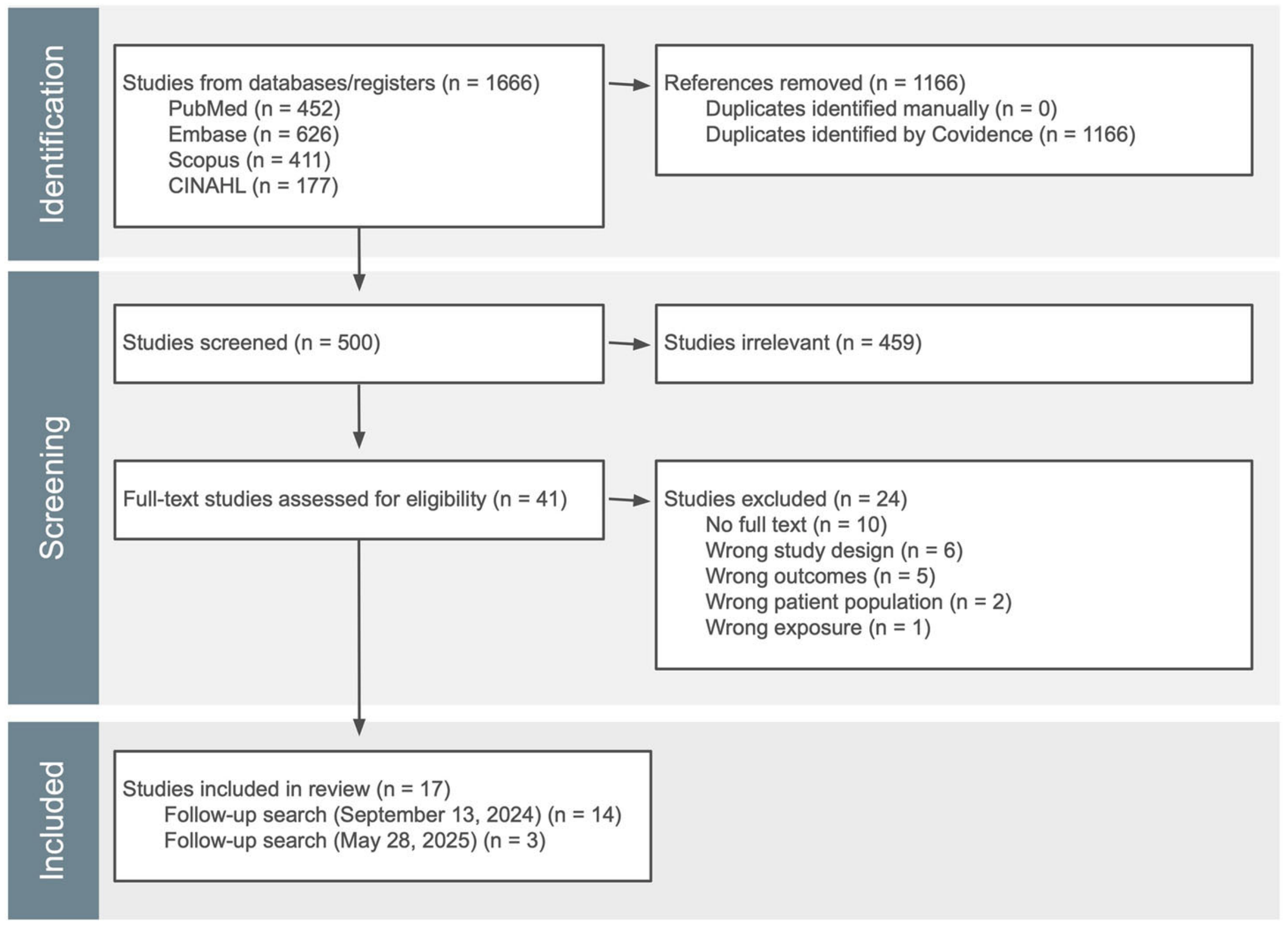
At the same time, a systematic review published in npj Digital Medicine examined telemedicine utilization patterns among patients with limited English proficiency across 17 studies in the United States. The findings reveal persistent disparities in virtual care access.
Among seven studies analyzing overall telemedicine utilization, five reported significantly lower utilization for patients with LEP compared to those with English proficiency. Five out of seven studies investigating telemedicine use compared to in-person visits found lower telemedicine utilization for LEP patients.
Most strikingly: all seven studies analyzing telemedicine by modality found significantly lower video use for patients with LEP than those with English proficiency.
Why this convergence matters now
Virtual care offers potential solutions to some of the barriers driving healthcare avoidance among immigrant populations. Telemedicine can reduce the visibility of seeking care, eliminate transportation concerns, and provide access from the safety of home — factors that matter when patients are weighing whether to engage with the healthcare system at all.
But these benefits only materialize if patients can actually access virtual care. And the evidence shows that LEP patients face compounding barriers that prevent them from utilizing telemedicine at the same rates as English-proficient patients.
The systematic review identified several factors contributing to lower telemedicine utilization among LEP patients: lack of video-compatible devices and reliable internet access, low digital literacy, limited interpreter availability for video visits, unfamiliarity with video-based healthcare platforms, and inadequate language support across telehealth systems.
When these barriers intersect with heightened fear and institutional distrust, the result is a population that needs virtual care options most but can access them least.
Click here to learn more about Martti’s telehealth-integrated interpretation.
The modality gap
The disparity in video versus telephone utilization is particularly notable. All seven studies in the systematic review that examined telemedicine modality found significantly lower video use among LEP patients compared to English-proficient patients.
This matters because video visits provide higher-quality, more interactive healthcare experiences than telephone-only consultations. Video enables visual assessments, non-verbal communication, and more effective patient-provider interaction — particularly important for specialties like cardiovascular care where visual assessment supports clinical decision-making.
Research suggests video visits are associated with better diagnostic accuracy, improved decision-making, and fewer medication errors than telephone visits. Yet LEP patients consistently default to telephone-only consultations or avoid virtual care entirely.
One study in the systematic review found that among patients with prior video visit experience, there was no significant difference between LEP and English-proficient patients in choosing video modality. This suggests that initial barriers — not inherent preference — drive the disparity.
The interpreter availability challenge
Several studies in the systematic review identified limited interpreter availability as a key barrier to virtual care access for LEP patients. In some cases, healthcare systems restricted non-English speakers to telephone-only telemedicine specifically because interpreter services weren't available for video visits.
This creates a troubling dynamic: the patients who most need high-quality interpretation to navigate complex medical conversations are systematically channeled toward lower-quality modalities — or avoid virtual care altogether.
Interestingly, one study found that when LEP was measured by documented need for an interpreter rather than language preference, telemedicine utilization patterns shifted. Patients with documented interpreter needs showed higher telemedicine utilization for both new and returning visits, suggesting that when interpretation services are reliably available and integrated into virtual care workflows, utilization barriers diminish.
Click here to learn more about Martti’s telehealth-integrated interpretation.
What language access programs need
The evidence points to several requirements for equitable virtual care delivery:
Interpreter services must be available across all telemedicine modalities
Restricting LEP patients to telephone-only visits due to interpreter availability creates a two-tiered system that undermines both care quality and health equity.
Integration matters
Interpreter services must work seamlessly across the platforms patients and providers are already using, such as Epic, Teladoc, eClinicalWorks, Zoom, Microsoft Teams, WebEx, Doxy.me, AmWell, and others. When interpretation requires separate systems or complex workarounds, it becomes a barrier rather than a solution.
Digital literacy support is essential
The systematic review found that lack of familiarity with video-based platforms contributes to lower utilization. Language access programs should consider how to support patients in navigating virtual care technology, particularly for first-time users.
Documentation and privacy protections must be clear
In an environment where 51% of immigrants worry about information sharing, transparent documentation of interpreter services, HIPAA compliance, and patient privacy protections becomes both an operational necessity and a trust-building tool.
Quality must be consistent across settings
Professional medical interpreters trained in healthcare terminology, ethical standards, and cultural context are critical for both in-person and virtual care — but particularly important in virtual settings where communication challenges are already heightened.
Moving forward
At Martti, we've built our platform to integrate directly with leading telehealth and EHR systems because we understand that interpreter services must meet patients where they are. When interpretation is embedded into the platforms providers and patients already use — rather than requiring separate logins, phone numbers, or coordination — it removes friction that can prevent LEP patients from accessing virtual care.
The intersection of rising healthcare avoidance and persistent telemedicine access barriers creates an urgent challenge for language access programs. Virtual care has the potential to address some of the fears driving immigrants away from healthcare, but only if LEP patients can access it with the same ease and quality as English-proficient patients.
For language access leaders, these findings underscore a strategic imperative: ensuring that interpreter services are not an afterthought in virtual care delivery, but an integrated component that enables equitable access across all modalities and platforms.